11 Paediatric donors
11.1 Paediatric donor suitability
All children who die in intensive care should be considered for potential organ donation.
The overall rate of organ donation in children is similar to that in adults; however, this rate declines below two years of age.1 This is due to a combination of factors – primarily medical unsuitability and age and weight limits for retrieval and transplantation.1 Corkery-Lavender T, Millar J, Cavazzoni E & Gelbart B. Patterns of organ donation in children in Australia and New Zealand. Crit Care Resusc, 2017; 19:296-302 ×
Clarity regarding donor eligibility criteria and allocation protocols is critical to maximising donation opportunities. Particularly in the context of paediatric donation, confidence that a potential donor has a good likelihood of being suitable for transplantation is an important factor in initiating the donation conversation. Work to optimise donor identification in paediatric and neonatal intensive care units is ongoing, and criteria continue to be refined regarding suitability for transplantation of organs from paediatric donors, particularly from the smallest of these donors.
The recommendations below reflect local and international experience and current evidence with respect to paediatric donation and transplantation. However, it is acknowledged that there is a spectrum of experience with respect to the transplantation of organs from small paediatric donors and not all units will feel it is appropriate to consider all donors according to the criteria below. In order to facilitate the pathway for donation and allocation of these organs, transplant units should develop their own protocols for acceptance of paediatric donors, guided by the recommendations below as well as local expertise and other relevant considerations.
11.2 Paediatric kidney donation and allocation
For donors aged greater than 5 years or greater than 20kg, kidney allocation should proceed as for adult donors. For donors >10kg to 20kg, or aged >1 to 5 years, standard allocation also applies, although kidneys should be offered en-bloc first, then subsequently as single kidneys.2,32 Singh A, Stablein D and Tejani A. Risk factors for vascular thrombosis in pediatric renal transplantation: A special report of the North American Pediatric Renal Transplant Cooperative Study. Transplantation , 1997; 63(9): 1263-1267. 3 Foss A, Gunther A, Line PD, et al. Long-term clinical outcome of paediatric kidneys transplanted to adults. Nephrol Dial Transplant , 2008;23(2):726-729. ×
Donors >5kg to 10kg or >3 to12 months constitute a broad category with varying implications for the complexity of retrieval and transplant surgery, particularly in the case of the smallest donors. Availability of appropriate surgical expertise will influence the utilisation of such donors. Ideally, these organs should be managed in centres with specialist experience in small grafts, where clear protocols exist on how to manage them. Centres should pre-emptively discuss their readiness and capacity to transplant small organs. Centres willing to transplant very small organs may also nominate one or more of their senior transplant physicians and surgeons to act as local experts to provide pre-allocation advice to donation staff.
Donor history should be reviewed at the time of pre-allocation discussion and subsequent organ offer, considering possible indications of inherited paediatric renal disease and/or complications of neonatal/paediatric ICU management. Given the relative lack of experience with retrieval and transplantation of very small organs, donor history and any potential risk factors should be documented and post-transplant outcomes carefully monitored. Regular audit of transplant outcomes associated with the donor criteria below will be important to assess their utility and validity and to build evidence-based criteria for the allocation of very small kidneys.
In addition to routine donor information, offers of very small paediatric donors should be accompanied with the following documented data:
antenatal factors: normal antenatal morphology scan, absence of oligohydramnios, absence of history of transmissible infection
gestational age at birth and/or reduced size for gestational age
renal ultrasound with details of kidney/ ureter/ bladder anatomy and kidney size percentile for age
presence of extra-renal congenital anomalies or syndrome with likelihood of systemic impact affecting the kidneys
renal function: creatinine with normal range for age and gestation
acute illness factors: history of central/ umbilical vascular catheterization +/- thrombosis.
Table 11.1: Recommendations for paediatric kidney donation (SK: single kidney, EB: en-bloc)

11.3 Paediatric liver and intestinal donation and allocation
Paediatric liver transplantation requires appropriate size matching. For very small infants requiring liver transplantation, a suitable donor may therefore include a very small paediatric donor. The lower size limit of potential donors includes neonatal donors.
Table 11.2: Recommendations for paediatric liver and/ or intestinal donation
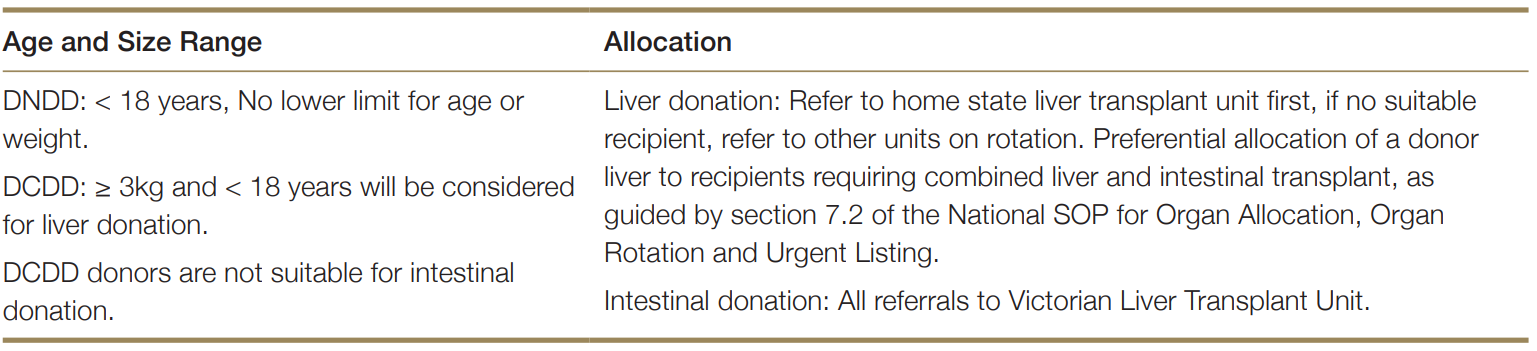
Paediatric donor livers must first be offered to paediatric recipients (<18 years of age). This is the case for whole liver or for both lobes of a split liver when the potential donor is less than 18 years of age. If there are no suitable paediatric recipients in the home state, it is then offered on national rotation for paediatric recipients.
Paediatric livers will only be considered for an adult recipient in two circumstances:
a. In the event that the paediatric liver rotation has been exhausted, the offer returns to the home state and the home state can allocate to an adult recipient. In the event that the home state do not have a suitable recipient, the liver is offered on the ADTCA/TSANZ Adult Liver Allocation Rotation – please see Appendix A of the National SOP for Organ Allocation, Organ Rotation and Urgent Listing.
b. There is a very sick/dying potential adult recipient in the donor home state. Allocation in this circumstance requires discussion and consensus by the Paediatric Liver Transplant Units Directors (or their delegate).
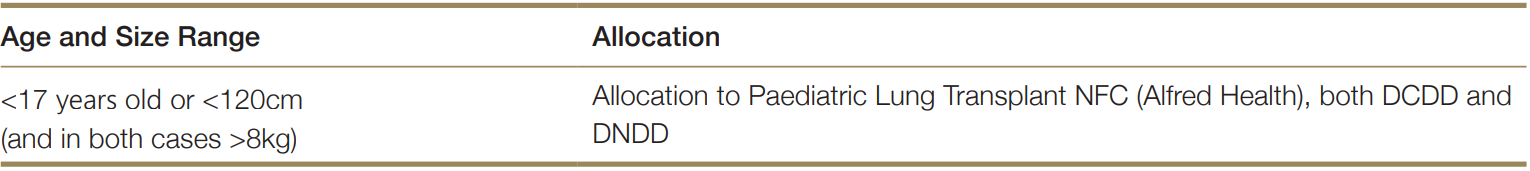
11.4 Paediatric lung donation and allocation
The recipient criteria are set out by the Nationally Funded Centre (NFC) for Paediatric Lung and Heart-Lung Transplantation and supports lung transplantation for children ≥4 years and >10kg. Reflecting that children this small may have restrictive lung disease and a small chest cavity, smaller paediatric donors may be suitable as per recommendations in Table 11.3.
Table 11.3: Recommendations for paediatric lung donation and allocation
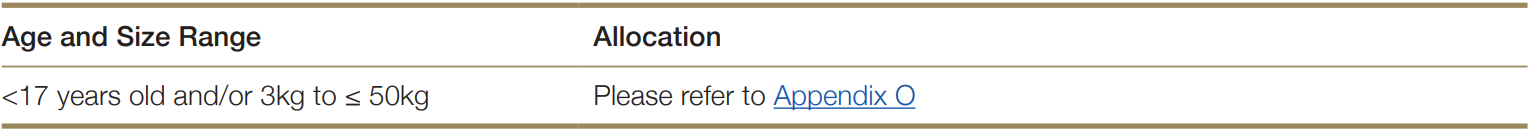
11.5 Paediatric heart donation and allocation
Infants and children can derive significant benefit from heart transplantation, with a median post-transplant survival of up to 25 years for infants.4 Any donor weighing greater than or equal to 3 kg is deemed potentially suitable. For infants with severe heart disease, an early decision on pursuing wait-listing for cardiac transplant vs mechanical support (VAD) is often necessary.5 An understanding of the size of the donor pool and likely waiting time is critical in informing this decision. Accordingly, it is recommended that all potential donors ≥3kg be formally assessed for heart donation. Discussion with the transplant team to determine if there is a suitable recipient should only be undertaken if this is the express wish of the donor family. A ‘paediatric donor heart’ is defined as being retrieved from a donor <17 years-old AND/OR 3kg to ≤50kg. The paediatric heart offering workflow process is outlined in Appendix O.4 Rossano JW et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Twenty-second pediatric heart transplantation report – 2019; Focus theme: Donor and recipient size match. J Heart Lung Transplant, 2019 Oct;38(10):1028-1041 ×5 Kirk R, Dipchand AI, Davies RR et al. ISHLT consensus statement on donor organ acceptability and management in pediatric heart transplantation. J Heart Lung Transplant. 2020 Apr;39(4):331-341. ×
Paediatric donors with both heart and lungs suitable for use as a bloc should be referred to the Paediatric Heart Lung Transplant Centre at the Alfred – see 11.5.1 below.
Table 11.4: Recommendations for paediatric heart donation and allocation
11.5.1 Paediatric heart-lung blocs and allocation
Infants and children with a variety of medical conditions may require heart-lung transplant (2-3 cases per year). Paediatric donors suitable for these children are rare and such transplants are only performed by the Paediatric Heart-Lung Transplant Centre (i.e. recipients under age 16) at the Alfred. The prioritisation and allocation of all these smaller donor organs must be considered at the time of referral as a bloc.
Table 11.5: Recommendation for paediatric heart-lung donation

11.6 Paediatric pancreas donation and allocation
Paediatric DNDD donors >25kg are suitable for pancreatic donation. These should initially be offered for solid organ donation and, if not allocated, then offered for islet donation.
Paediatric DCDD donors are not currently suitable for pancreas donation.
Table 11.6: Recommendations for paediatric pancreas donation
